Part 2, Strategy 4
Action Item 2: Ensure sufficient availability of treatment and programs.
Why it matters
All state and local governments face some degree of difficulty connecting people on supervision to effective treatment and programming. Because individual needs vary substantially, a one-size-fits-all approach to providing treatment and supports is not effective and can be a poor use of critical resources. Prioritizing resources for people who are at the highest risk of reoffending and integrating services and supervision to address those risks and needs will deliver the best outcomes. State and local policymakers can help ensure sufficient availability if they invest in effective treatment and programming, increase the provider workforce, and train providers to work with people on supervision.
Far too often, behavioral health care providers do not have the necessary specialized knowledge and training on evidence-based practices to provide effective treatment to people in the criminal justice system. A further complication is that existing health care reimbursement rates may not adequately compensate treatment providers for the higher costs often associated with providing effective services for people in the criminal justice system, often resulting in providers’ unwillingness or inability to work with this population.
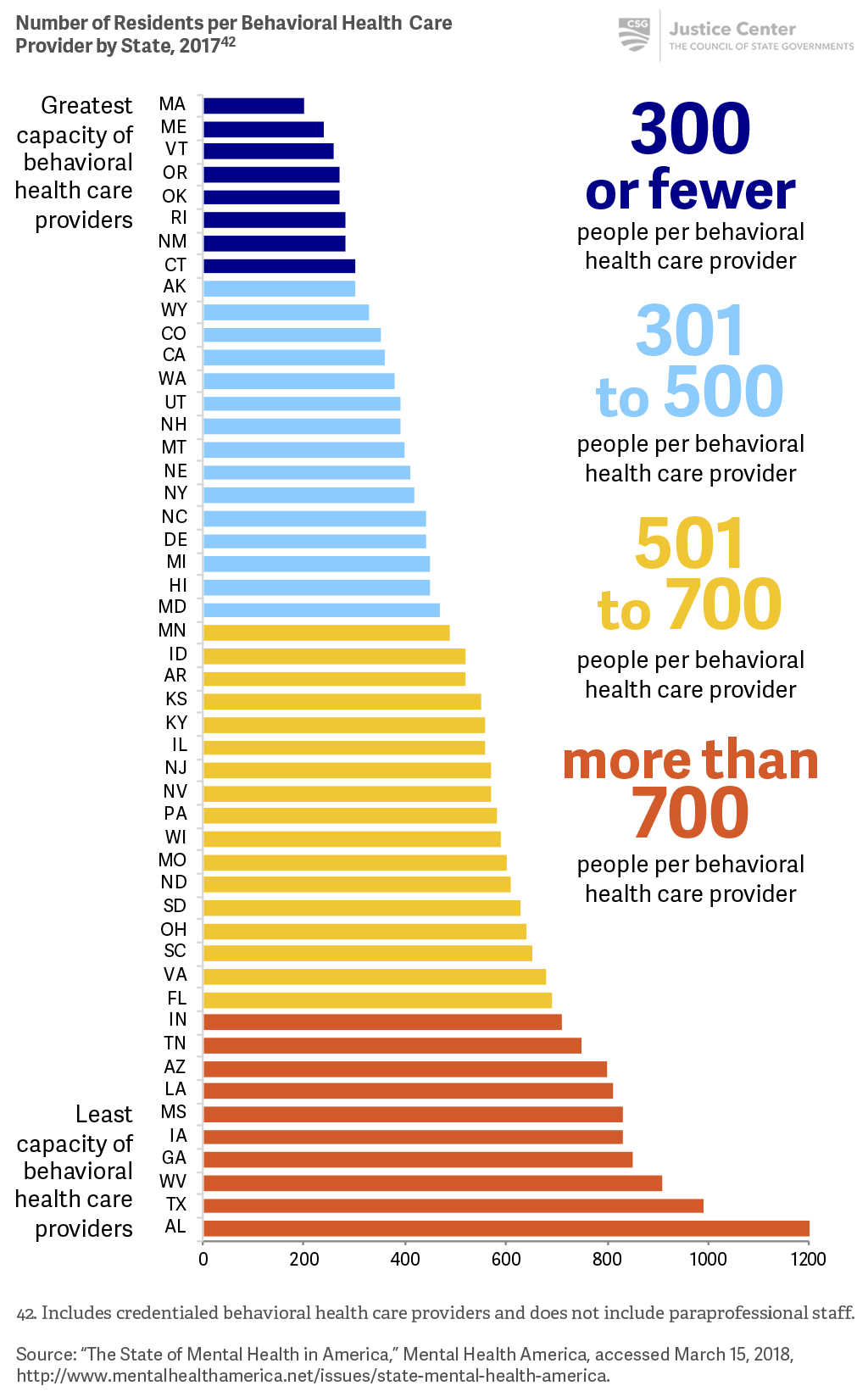
A shortage of community treatment options and qualified providers impedes people’s access to needed services that, when combined with effective supervision, are proven to reduce recidivism. States often find they need to expand the number of licensed professionals providing treatment interventions, as well as increase the number of paraprofessionals, such as peer support specialists, recovery coaches, case managers, and care coordinators offering recovery-based services. An assessment of needs and available resources can also help policymakers develop strategies to enlarge capacity and quality of services—such as ensuring adequate reimbursement rates for treatment providers and offering performance incentives—to increase the availability of treatment and services. (For additional information on ensuring that a range of behavioral health services are available for people in the criminal justice system, see Part 1, Strategy 2.)
What it looks like
- Evaluate the need for programming and treatment and compare to current capacity.
- See Case Study: States invest in programs needed to reduce recidivism
- Prioritize intensive services for people who have the highest risk of reoffending and greatest criminogenic needs.
- Invest in high-quality treatment and programs that address multiple needs.
- Develop payment strategies that incentivize treatment providers to deliver specialized services for the criminal justice population.
- Expand the pool of treatment providers trained to work with the criminal justice population.
- See Case Study: Nebraska improves collaboration between treatment providers and corrections agencies
- Expand the paraprofessional workforce, as needed.
- See Case Study: Kansas adds peer support specialists and recovery coaches to probation offices
- Use performance incentives to ensure availability and quality of services.
Key questions to guide action
- Does your state assess the availability of treatment and programming for people on supervision?
- How does your state determine necessary funding levels to meet the needs of people who are at the highest risk of reoffending?
- What steps is your state taking to increase the number of treatment providers and paraprofessionals who are trained to work with people in the criminal justice system?
- Do supervision agencies use performance incentives with community-based programs or treatment providers? What incentives and practices are used to ensure that people remain in treatment?
- How can your state support local efforts to increase the availability of treatment and programming for people on supervision?
Use the information that follows to inform your answers to these questions.
To ensure sufficient availability of treatment and programming, states need to provide appropriate funding, expand the pool of qualified service providers, and require training.
The capacity of behavioral health care providers varies from state to state.
Case Study
States invest in programs needed to reduce recidivism
Some states have invested a significant amount of money in ensuring that people on supervision receive the range of services they need.
- At a time when budgets were cut dramatically amid a fiscal crisis, Alabama’s legislature appropriated $31 million between FY2016 and FY2019 to expand treatment and programming for people on supervision.
- West Virginia invested more than $11 million between FY2014 and FY2017 to expand addiction treatment and services for people on probation or parole. Substance use is a leading factor for people who fail to meet the conditions of supervision, and services provided through the grants are prioritized for people most likely to reoffend. State agencies are ensuring that new resources for treatment are leveraging Medicaid and other health insurance coverage for behavioral health services.
While no state has closed the gap in funding needed to provide treatment and programming to people on supervision, some states conduct analyses to identify how much funding is necessary to provide needed programs and treatment for those who are most likely to reoffend. Idaho requires its Department of Corrections and Department of Health and Human Welfare to submit a joint report to the legislature each year analyzing the criminogenic needs of people on probation and parole; current funding available to deliver effective, evidence-based programming to address those needs; and additional funding required to meet the behavioral health treatment needs of all moderate- and high-risk people on supervision.
Case Study
Nebraska improves collaboration between treatment providers and corrections agencies
Funding and increasing capacity alone aren’t sufficient to guarantee quality treatment and programming. States also need to ensure that service providers are trained to work with people on supervision and that service providers and supervision agencies improve collaboration to reduce gaps in services. Nebraska’s statewide probation agency created a system to register approved service providers that can service people on probation. This system ensures quality of services by requiring community-based behavioral health providers to be trained on evidence-based practices for people on supervision and to use up-to-date assessments and counseling techniques. Service providers use a secure probation portal to share all assessment information and monthly progress reports with probation officers. The registered service provider program streamlines processes by permitting electronic referrals for services and standardizes assessments and reporting. The system also ensures collaboration and communication between community supervision officers and service providers, requires ongoing training and quality controls between the Office of Probation Administration and service providers, and allows the Office of Probation Administration to track behavioral health needs and treatment across the state.
Case Study
Kansas adds peer support specialists and recovery coaches to probation offices
To help connect people to services quickly or provide support while they wait for treatment, Kansas added peer support specialists and recovery coaches to probation offices to attend to people with mental illnesses and addictions, respectively.
Paraprofessional services can be Medicaid reimbursable and, while they cannot replace professional assessment and treatment services, are relatively inexpensive and add value in other ways. Paraprofessionals can help people who have completed treatment sustain their recovery, navigate complex health care systems, and engage people in services that function as a helpful “stopgap” when they are waitlisted for treatment. These trained specialists and coaches are people who have “lived experience” overcoming problematic substance use or battling mental illnesses themselves. They work to promote hope, motivation, and dedication in their clients and prevent relapse during the recovery process.
